Chronic Ankle Instability
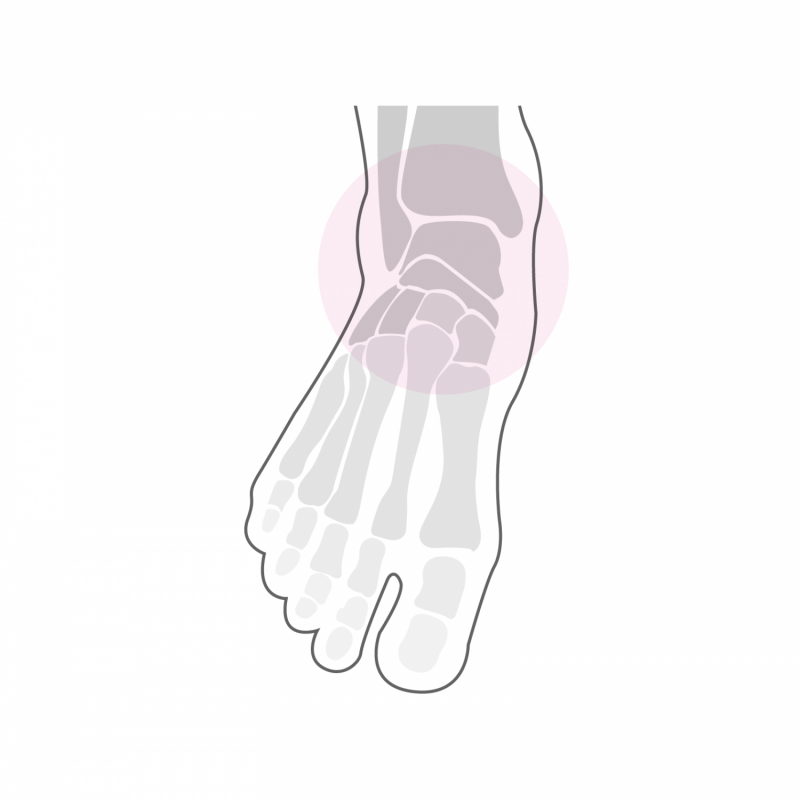
Chronic ankle instability is caused by failure of the main ankle ligaments following repeated sprains. It is most often the external ligaments of the ankle that are affected, but chronic instability of the internal ligaments can also occur especially following complex sprains of the ankle. This instability of the ankle is manifested by a feeling of "laceration" in the ankle, even during normal walking in conventional shoes. This results in repeated sprains and the development of chronic pain mainly located on the external side of the ankle. If the peroneal tendons are affected, there is often a persistent painful swelling just below the external malleolus. The pain is first present on exertion, then can settle at rest depending on the anatomical structures concerned.
The diagnosis is primarily made by clinical examination of the ankle which highlights the insufficiency of ligaments. There is an abnormal “opening” of the ankle laterally and the tensioning of the peroneal tendons against resistance is limited and painful. A radiological assessment must be carried out in search of possible old bone lesions, early osteoarthritis and an osteochondral lesion (partial lesion of the articular cartilage and the underlying bone).
Treatment
The treatment is conservative at first with the aim of improving muscle function by strengthening exercises and proprioception exercises (balance exercises on the injured foot on a flat surface, then on unstable trays). A support splint to wear while playing sports and adapting activities often helps to stabilize the situation and relieve pain.
If, despite this conservative treatment, the symptoms persist, surgical treatment aimed at restoring the anatomy at the level of the injured ligaments makes it possible to treat the instability. Depending on the anatomy of the hindfoot, this ligament reconstruction is associated with a correct osteotomy of the calcaneus, possibly a correct osteotomy of the 1st metatarsus and a gesture on the peroneal tendons (direct suture or tendon transfer). In the event of an osteochondral lesion, arthroscopic debridement of the lesion, associated with the placement of a bone graft taken from the proximal tibia makes it possible to treat this problem at the same operating time.
The intervention can last up to two hours depending on the gestures to be performed and can be performed under general or spinal anesthesia. It can be combined with local anesthesia of one of the main nerves of the foot (popliteal block), which significantly reduces post-operative pain. It takes two to three nights of hospitalization. Walking is done immediately from the first post-operative day in full discharge of the foot operated using canes in a removable plastered boot. This total discharge must be observed during the first two weeks. The removal of stitches and the making of a new removable plastered boot take place 2 weeks after the intervention. From this moment, a partial load of 15 to 20 kg on the operated foot is allowed, this for 4 additional weeks. A clinical and radiological check-up is carried out 6 weeks after the operation.
In case of sufficient bone healing, a gradual increase in the load on the foot is done over a period of two to three weeks until the total load. From the 7th week, a physiotherapy treatment aimed at reducing the swelling of the foot and improving its function is implemented. Resumption of activities such as swimming, cycling or moderate walking is possible from the 10th post-operative week. More restrictive activities on the foot such as longer hikes can be considered from the 7th month after the intervention. Activities such as running or other stop and go sports are not recommended after this type of intervention. The foot will continue to refine and heal until one year post-operatively and gradually regain its full function. Wearing a suitable plantar support is recommended later to maintain the correction.
